Turkey meat allergy is rare but can cause concerning symptoms in some people. As with other food allergies, understanding the causes, symptoms, diagnosis and management is key for those affected This article provides an in-depth look at turkey meat allergy
What Causes Turkey Meat Allergy?
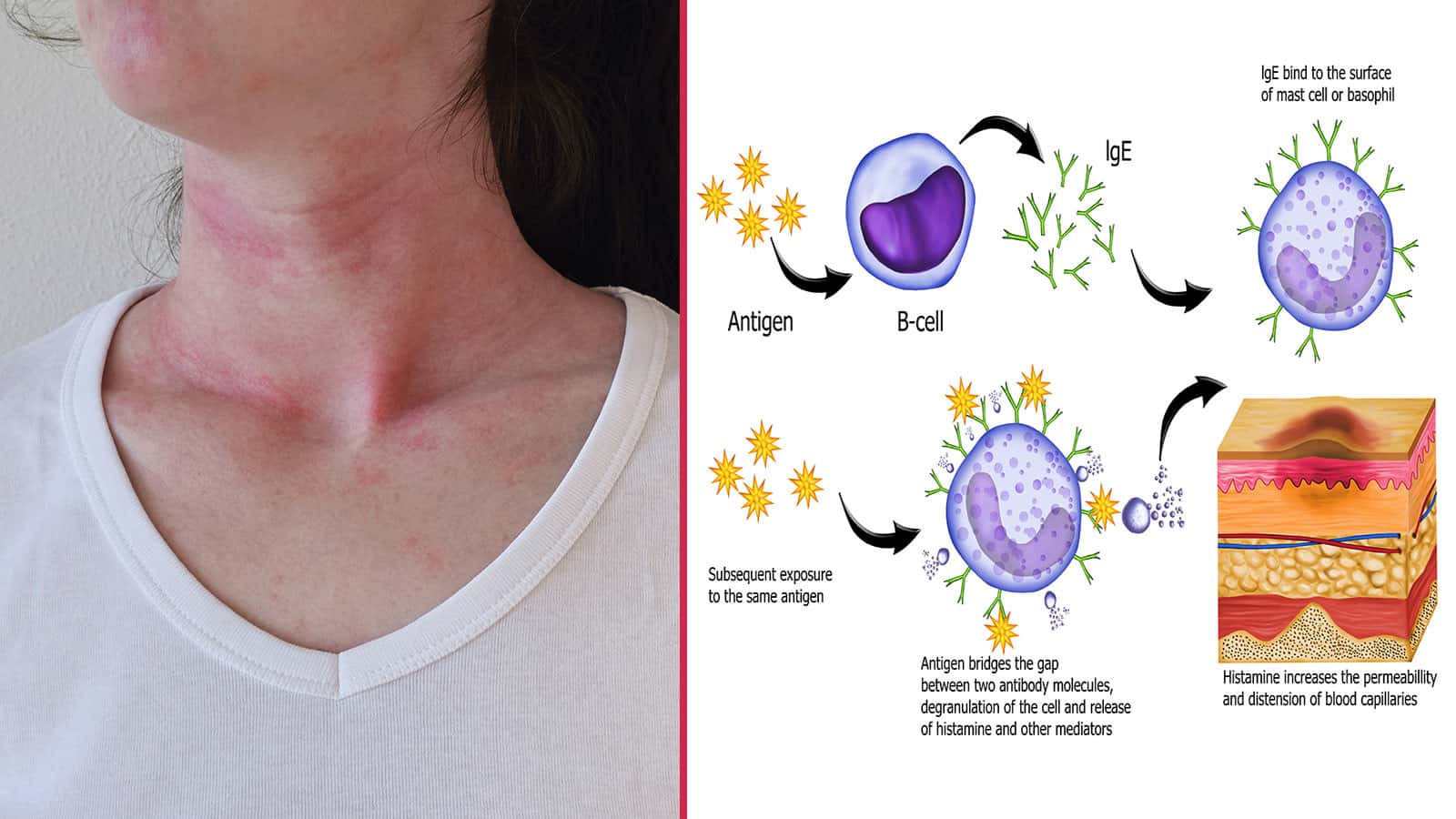
Turkey meat contains proteins that can trigger an allergic response in sensitive individuals. The immune system mistakenly identifies these harmless proteins as dangerous invaders and releases antibodies like immunoglobulin E (IgE) to attack them.
Cross-reactivity with chicken or other poultry is common, as they share similar protein structures. Tick bites can also introduce allergenic sugars like alpha-gal into the body, inducing sensitivity.
While the underlying cause is unclear, risk factors like genetics, other food allergies or skin conditions may contribute Turkey meat allergy can develop at any age
What Are the Symptoms of Turkey Meat Allergy?
Symptoms usually occur within minutes to hours after eating turkey and can range from mild to severe:
- Oral allergy syndrome – itching or tingling in the mouth
- Hives, rash or itching on the skin
- Stomach pain, nausea, vomiting, diarrhea
- Swelling of the lips, face, tongue and throat
- Wheezing, nasal congestion, trouble breathing
- Anaphylaxis – a life-threatening reaction affecting multiple body systems
Skin and digestive symptoms are most common. Severe anaphylaxis is possible but less frequently seen.
How is Turkey Meat Allergy Diagnosed?
Diagnosing turkey allergy involves:
- Skin prick test – Pricking the skin with turkey extract to look for a localized reaction
- Blood test – Measuring turkey-specific IgE antibody levels
- Elimination diet – Removing turkey from the diet to see if symptoms improve
- Oral food challenge – Eating turkey under medical supervision to confirm an allergy
Testing is the only way to definitively diagnose a turkey meat allergy. Inform your doctor if you suspect this allergy.
What is the Treatment for Turkey Meat Allergy?
The main treatment is strict avoidance of turkey meat and products containing it. Carefully read ingredient labels and be cautious when dining out. Epinephrine auto-injectors like EpiPens should be carried in case of anaphylaxis.
Antihistamines can provide relief from mild allergic reactions. See an allergist for other medical management options. Desensitization therapies are being researched but are not yet widely available.
Living with Turkey Meat Allergy
Having a turkey allergy requires vigilance around food and emergency preparedness. Here are some tips:
- Check labels for turkey broth, oil, gelatin and other derivatives
- Notify wait staff of the allergy when eating out
- Carry epinephrine if you are at risk for anaphylaxis
- Wear a medical alert bracelet to identify the allergy
- Educate friends and family members on recognizing allergic reactions
- Find healthy, tasty alternatives like fish, beans, tofu or beef
While turkey allergy can be challenging, being informed and proactive helps ensure safety and enjoyment at mealtimes. See an allergist if you suspect this allergy so proper precautions can be taken.
Key Takeaways on Turkey Meat Allergy
- A rare but potentially serious food allergy triggered by proteins in turkey meat
- Can cause skin, respiratory, gastrointestinal and cardiovascular symptoms
- Diagnosis requires skin or blood tests; strict avoidance is the main treatment
- Carrying epinephrine is vital for people at risk of anaphylaxis
- Careful label reading, substitutions and alerting others helps minimize risks
Understanding the signs, testing options, and prevention techniques for turkey meat allergy aids in safely navigating this condition. Being prepared helps minimize risks and dietary limitations. Consult an allergist to get proper testing and advice if you suspect this allergy.
Managing a severe food reaction with epinephrine
A food allergy, including a meat allergy, can cause symptoms that range from mild to life-threatening; the severity of each reaction is unpredictable. People who have previously experienced only mild symptoms may suddenly experience a more severe reaction, including anaphylaxis. In the US, food allergy is the leading cause of anaphylaxis outside the hospital setting.
Epinephrine is the first-line treatment for anaphylaxis, which results when exposure to an allergen triggers a flood of chemicals that can send your body potentially into shock if not treated promptly. Anaphylaxis can occur within seconds or minutes, can worsen quickly, and can be deadly.
Once you’ve been diagnosed with a food allergy, your allergist will likely prescribe an epinephrine auto-injector and teach you how to use it. Check the expiration date of your auto-injector, note the expiration date on your calendar, and ask your pharmacy about reminder services for prescription renewals.
If possible, have two epinephrine auto-injectors available, especially if you are going to be far from emergency care, as the severe reaction may reoccur. Epinephrine should be used immediately if you experience severe symptoms such as shortness of breath, repetitive coughing, generalized hives, tightness in your throat, trouble breathing or swallowing, or a combination of symptoms from different body areas such as hives, rashes, or swelling on the skin coupled with vomiting, diarrhea, or abdominal pain.
Even if you are uncertain whether a reaction calls for epinephrine, you should use it, as the benefits of epinephrine far outweigh the risk.
Common side effects of epinephrine may include anxiety, restlessness, dizziness, and shakiness. If you have certain pre-existing conditions, you may be at a higher risk for adverse effects with epinephrine.
Your allergist will provide you with a written emergency treatment plan that outlines which medications should be given and when.
Once epinephrine has been administered, immediately call 911 and inform the dispatcher that epinephrine was given.
Other medications may be prescribed to treat symptoms of a food allergy, including antihistamines and albuterol, but it is important to note that there is no substitute for epinephrine: It is the only medication that can reverse the life-threatening symptoms of anaphylaxis. These other medications can be given after using epinephrine, and antihistamines alone may be given for milder allergic reactions per your food allergy action plan.
Can You be Allergic to Meat??
FAQ
What are the symptoms of turkey allergy?
What is the most common meat allergy?
How do you know if you have a meat intolerance?
Will turkey trigger chicken allergy?
Do you have a meat allergy?
A meat allergy can develop any time in life. If you are allergic to one type of meat, it is possible you also are allergic to other meats, as well as to poultry such as chicken, turkey and duck. Studies have found that a very small percentage of children with milk allergy are also allergic to beef.
Is Turkey lethargy a symptom of an allergy?
Many attribute this lethargy to the turkey eaten on Thanksgiving. Many feel that they are having an allergic reaction to turkey due to this somnolence, however, it is not an allergy at all. Allergies to turkey meat are not common, but a true allergy to turkey can occur in some individuals.
Is there a link between meat allergies and other foods?
Researchers have found a number of links between meat allergies and other foods too, especially with a primary beef allergy (not caused by alpha-gal). Beef allergy in children who have a cow’s milk allergy may be found in up to 20% of cases.
Can you eat beef if you have a chicken allergy?
People who can’t eat beef may not be aware that meat from sheep can cause symptoms, and chicken allergies may really be due to a cross-reaction caused by fish allergy. Researchers have found a number of links between meat allergies and other foods too, especially with a primary beef allergy (not caused by alpha-gal).
